|
Here are several postings from Dr.McDougall's newsletter:
Type-2 Diabetes – the Expected Adaptation to Overnutrition
Sixteen million people in the United States have type-2 diabetes, which
shortens lifespan by up to 15 years, leads to almost 300,000 deaths annually, and costs about $100 billion annually.
Since 1980 the incidence has increased by
30%. Born in the year 2000, your male child’s lifetime risk of developing
type-2 diabetes is nearly 33%, and a female’s risk will be 39% when following the Western diet. Worldwide,
135 million people have type-2 diabetes and by 2025 the incidence is predicted to reach 300 million people worldwide.
This form of diabetes was once referred to as “adult-type diabetes”
because in the past, type-2 diabetes was rare in children. However, over the last two decades, there has been a 10-fold increase
in incidence of type-2 diabetes in children, because of the rapidly growing numbers with obesity from an escalating exposure
to rich foods, compounded by a lack of exercise.
The general state of poor health of Westerners, as reflected by diabetes,
escalates unchecked for 3 important reasons:
1) This growing epidemic of type-2 diabetes and obesity is fueled by
huge profits generated by a food industry super-sizing everything by stuffing their irresistible morsels with fat, sugar,
refined flour, and calories.
2) Medical doctors continue to prescribe remedies that have never
cured a single case of diabetes. Furthermore, the usual “poly-pharmacology” of medications they rely
upon promotes weight gain, heart disease, and hypoglycemia, along with other serious adverse effects. From all these
expensive medications there is a small reduction in complications, such as kidney and eye damage, which still fails to offset
the tremendous harm done by their efforts.
3) The American Dietetic Association has remained steadfast in
their recommendation of a portion-controlled version of the Western (American) diet – an impossible diet to follow (because
of its complex rules and semi-starvation nature) – made up of ingredients, like fat, sugars, refined foods, and cholesterol,
that caused the patients’ problems in the first place.
In 1927 Dr. E. P. Joslin, founder of the famous Joslin Diabetic Center
in Boston, suspected a high-fat, high-cholesterol diet might favor the development of diabetes and its major complication,
atherosclerosis. He prophetically wrote: “I believe the chief cause of premature atherosclerosis in diabetes, save for
advancing age, is an excess of fat, an excess of fat in the body (obesity), an excess of fat in the diet, and an excess of
fat in the blood. With an excess of fat diabetes begins and from an excess of fat diabetics die, formerly of coma, recently
of atherosclerosis.” And now, 75 years after Joslin’s farsighted message, diabetes is the fastest growing
disease in the world.
 Type-2 Diabetes: A Runaway Epidemic Caused by Rich Foods Type-2 Diabetes: A Runaway Epidemic Caused by Rich Foods
The cause of this skyrocketing health tragedy is easily seen by observing
everyday people striving for the “good life.” Feasting from the king’s table brings on the diseases
of royalty, like obesity, gout, and diabetes. Worldwide, the incidence of type-2 diabetes increases in direct proportion
to the consumption of meat, dairy products, sugars, fats, and calories by the residents. Type-2 diabetes has taken the
greatest toll on “minority” populations brought to the Western diet by migration to cities and giant industries
providing cheap fast food.
Native Americans, for example the Pima Indians of Arizona, introduced
to the Western diet over the past 75 years, are now afflicted so severely that as many as one-half of them has diabetes. However,
their genetic cousins, the Tarahumara Indians of Mexico, following a diet consisting of 90% corn and pinto beans (chili),
and vegetables (like squash), are free of type-2 diabetes – as well as obesity and heart disease. Similar dramatic
rises – from immunity to epidemic proportions – of type-2 diabetes have been seen in other people like Africans,
African-Americans, Mexicans, Chinese, and Polynesians, as they adopt the Western diet with enthusiasm. There are no exceptions
to this observation that when populations of people following a starch-based diet (rice, corn, potatoes, sweet potatoes, etc.),
switch to a diet of rich foods – meats, dairy products, added oils, and refined foods – they become overweight
and diabetic, and develop heart disease, breast, prostate and colon cancers, gallbladder disease, arthritis, multiple sclerosis,
and bowel problems. No exceptions!
Diabetes Is an Adaptive Response to Overnutrition
The malnutrition caused by the high-fat, low-fiber
Western diet places serious burdens on the body and requires it to make adaptions in order to survive under adverse conditions.
The calories consumed in excess of our needs cause us to gain fat – this is a natural, expected change. Soon a
point is reached when this accumulation becomes counterproductive – a point when any further excess body weight is likely
to cause serious physical harm. When this hazardous excess is reached, the body puts “the brakes on”
in order to slow the rate of gain. This is accomplished by a variety of changes that cause the hormone insulin to become
less potent. In other words, our cells become resistant to the actions of the fat-gaining hormone, insulin
– a state referred to as “insulin resistance.”
One of insulin’s primary jobs is to push fat
into the fat cells – thus saving fat for the day when no food is available (which for Westerners never comes). If
it were not for the adaptive mechanisms which allow for the development of “insulin resistance,” people would
commonly expand until they became so large that they could not get out of bed or fit through a doorway – a very rare
condition that does occur in 1000-pound sized people who need a forklift to move them to the hospital. (They make headlines
in the newspaper.)
One of insulin’s other important jobs is to
let sugar into the body’s cells – with a state of “insulin resistance” the sugar cannot get into the
cells easily – so it rises in the blood. The hallmark of the diagnosis of diabetes is an elevated blood sugar above
normal (usually normal is below 115 mg/dl fasting). With impotent insulin, the calories of fat and sugar we consume
cannot easily enter the cells; the body is essentially starving itself from the inside in a desperate attempt to compensate
for the overfeeding coming from the outside. To further reduce the burden of obesity, the body eliminates calories by
allowing sugar to spill over into the urine, like water falling over a dam. At this stage sugar is found with a urine
test – another common way to diagnosis diabetes. Most doctors and patients view the elevated blood sugar as the
enemy to be beaten down with medications – the result is a fat, sickly patient with a slightly lower blood sugar.
The Reason Medical Therapy Should Be
Your Last Choice
Diabetic medications have never cured anyone of
diabetes and actually compound the patients’ problems. The patient goes to the doctor, is diagnosed with diabetes,
placed on medication, and told to lose weight. Unfortunately, these medications make insulin more effective, causing
more fat to be stored in the fat cells. The average initial weight gain when diabetic medications are started is 8 to 20 pounds
– due to partially counteracting the protective effects of “insulin resistance.” Thus the well-behaved
patient takes the medications as directed, but then gains weight, and as a result of the added weight his diabetes becomes
worse. The patient returns to the doctor, is given a firm scolding for gaining weight, and then more medications are
prescribed because his sugars are even higher than before – this additional medication makes the patient even fatter
and the diabetes more out of control. The vicious cycle continues – and the patient and doctor are left guilt-ridden
and confused about their obvious medical failure. After all, they followed the pharmaceutical company’s instructions
exactly. Worse yet, the patients are not one bit healthier from all this effort and expense.
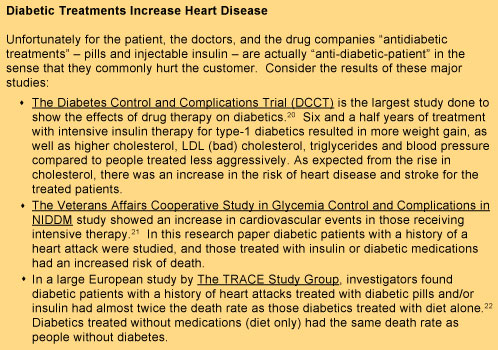
More than 30 years ago, when I was in medical
school, I remember doctors arguing about the benefits from aggressive use of medication to make the blood sugars lower, a
practice referred to as “tight control.” Ideally, keeping the blood sugars close to normal makes sense,
but in real life more harm than good is done for type-2 diabetics. First of all, no matter how hard the patient and
the doctor work at their goal, the blood sugar readings are all over the place – one test shows 60 mg/dl and the next
260 mg/dl. Soon it becomes obvious to the patient that the short-term goal of “normalizing” the blood sugar
levels is impossible using medications.
The next carrot held out is for long-term benefits:
preventing complications later in life. In truth, studies have shown there is some benefit for the eyes and the kidneys
with better control of blood sugar (especially for type-1 diabetics). However, the major threat to the life of
a diabetic is from heart attacks and strokes – diseases of the large blood vessels. Intensive medical therapy
using the most high-tech drugs to lower blood sugars has failed to reduce the risk for, and improve survival from, these two
major killers. In fact, the medications used to combat sugar will actually create more sickness and death from heart disease.
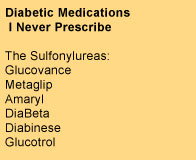
Since the early 1970s every single edition of the
Physician’s Desk Reference, found in every doctor’s office, has carried this warning in heavy back print
for their diabetic medications: “SPECIAL WARNING ON INCREASED RISK OF CARDIOVASCULAR MORTALITY.” The most commonly
prescribed diabetic medications, known as sulfonylureas,* cause fundamental changes in the function of cells that increase
the risk of heart attacks. These drugs, which are called “antidiabetic agents” by the pharmaceutical companies,
have recently been shown to more than double the risk of heart attacks and almost triple the risk of early death in patients
after an angioplasty. I never prescribe this type of diabetic pills, and always ask my patients to
stop them. All diabetics should be actively looking for a better approach – and so should any doctor interested
in his patients’ welfare.
The Treatment of Type-2 Diabetes with a Low-Fat,
Plant-Food Diet
Multiple studies dating as far back as the 1920s have shown the benefits
of a high-carbohydrate, low-fat diet in the treatment of type-2 diabetes. For example, studies from the University
of Kentucky Medical School reported as many as two-thirds of diabetics were able to discontinue insulin and almost all stopped
oral agents. A recent thorough review of the use of a vegetarian diet in the treatment of type-2 diabetes was published in
the September 2003 issue of the American Journal of Clinical Nutrition. In this review article Dr. David Jenkins reported
on research showing improvements in blood sugars in diabetics with 39% stopping insulin and 71% stopping diabetic pills after
three weeks of therapy. Relief of diabetic neuropathy pains, reduced lipids (cholesterol and triglycerides), and weight loss
have also been reported with a low-fat, pure-vegetarian diet. Another recent research paper has reported similar findings
with a low-fat vegetarian diet. Many of these people with type-2 diabetes are cured of their disease within three weeks,
and most will be cured of their diabetes over time as they adhere to a low-fat, high carbohydrate diet, exercise, and lose
all of their excess body fat.
This same kind of diet (in large part because of the restriction of animal
protein) has been shown to dramatically improve the health of the kidneys of diabetics (protein in the urine, a sign of diabetic
kidney damage, decreases and disappears). Research has also shown diabetic damage found in the
eyes (retinopathy) can be reversed with a low-fat diet. It’s interesting how kidney and eye damage, the two purported
benefits from drug therapy, are actually better treated with diet than with medications, at no cost and no side effects. A
low-fat vegetarian diet has also been shown to reverse heart disease (atherosclerosis), the number one killer of diabetics.
Many other researchers have praised a low-fat vegetarian diet as the best approach to prevent and treat most diseases that
plague people in modern societies, including people with diabetes. Possibly the most important effect of this dietary approach
(combined with exercise) is the scientifically established fact that this is the easiest and most effective way to lose weight
permanently. Obesity is the underlying cause of diabetes.
Practical Steps to Cure Type-2 Diabetes
If you are one of the millions of diabetic patients
facing a hopeless future of worsening diabetes, obesity, loss of vision, kidney failure, heart attacks, strokes, gangrene,
and early death and disability – even though you have visited your doctors regularly, and taken your medications faithfully
– then it is time to break this downhill spiral by changing your diet and exercise program. At the same time ask
your doctor to provide you with sensible, conservative, care. I do the following with my patients:
1) Stop diabetic pills and reduce
or eliminate insulin. In most cases, I have my patients stop all of their diabetic pills the day they start the McDougall
diet and exercise program and/or at least half of their insulin. If this reduction is not made in a timely manner, then
they run a real risk of developing hypoglycemia (too low blood sugar). I increase or reduce medications based on the
patient’s response and as a general guideline I try to keep their blood sugars between 150 to 250 mg/dl while I am trying
to adjust their medication needs. Stopping and/or reducing the medications reverses the weight gain immediately.
(Insulin cannot be stopped in type-1 diabetes, but the dosage is often reduced.)
2) Change them to a low-fat, high-fiber, plant-based
diet: the McDougall diet. The diet should be based around starches with the addition of fruits and vegetables –
there are no added vegetable oils. Sample foods are: oatmeal, whole wheat pancakes or potatoes for breakfast.
Lunch can be soups, salads, and sandwiches. And dinner may be thought of in terms of ethnic dishes, like Mexican burritos,
Chinese Mu Shu vegetables, Thai curried rice, or Italian whole grain pasta.
3) Ask them to exercise. Start at
a comfortable level and gradually build up. Exercise should be increased to the equivalent of at least a half hour of
walking a day.
4) Check their other risk factors for indications
of serious disease, such as cholesterol, triglycerides, and blood pressure. Then make diet and lifestyle modifications
to correct these (for example, fewer fruits and juices with high triglycerides and cholesterol, and less salt with high blood
pressure).
5) Have them take appropriate medications only.
For example, I prescribe:
-
· Small doses of insulin for too much weight loss or if my patient develops symptoms of diabetes, like too
frequent urination or excessive thirst.
-
· Cholesterol (and triglyceride) lowering medications in order to reach ideal levels of 150 mg/dl, especially
for patients at high risk for a stroke or heart attack. (See my September 2002 and June 2003 Newsletters.)
-
· Blood pressure lowering medications, are sometimes indicated in high-risk patients whose blood pressure
remains at 160/100 mm Hg or greater for months. (See my August 2002 Newsletter.)
A prescription of a low-fat diet and exercise can
be taught by any interested physician or dietitian. Most diabetics respond within days – and with continued weight
loss, most can be expected to stop all diabetic medications – and regain lost health and appearance. The most difficult
task for people with diabetes is to break from tradition – the following words may help. “The diet recommended
by the American Diabetic Association virtually guarantees all diabetics will remain diabetic,” claimed the pioneer nutritionist,
Nathan Pritikin, 30 years ago. His experiences from treating thousands of people with this disease convinced him that
type-2 diabetes is largely curable by following a healthy diet and moderate exercise. Obviously the failure of modern
diabetic management has been known long before most diabetics developed their disease – yet nothing changes for the
better. Your only chance is to rebel against commonly accepted advice. Don’t you think a revolt is long
overdue based on the poor results you have experienced so far?
Glycemic Index – Not Ready for Prime Time
“Every time I hear about glycemic index I want to puke,” complains
Tiffany, one of my nutritionally-oriented friends. “Then I ask the person who is telling me how bad potatoes are if
they even know what glycemic index means. They usually tell me glycemic index means the food is high in sugar.”
Sugars actually have a very low glycemic index (GI), and according to
the popular practice of judging foods based solely on GI, you would be making healthier choices by eating chocolate cake,
instead of carrots—or cheese-topped pizza, rather than potatoes. Candies and ice cream, because of their high
simple sugar and fat content, are absorbed from the gut into the body slowly; therefore these widely acknowledged “junk
foods” have lower GI values than so-believed “health-foods,” like whole grain breads and brown rice.
|
Low GI Doesn’t Necessarily
Equate with Healthy1 |
|
Junk Foods with GI less
than 40 |
Healthy
Foods with GI greater than 80 |
|
Chocolate Cake (38) |
Nabisco Shredded Wheat (83) |
|
Nestle Quick Strawberry Drink (35) |
Corn Meal Porridge (109) |
|
No Bake Egg Custard (35) |
Jasmine Rice (109) |
|
Sara Lee Premium Ice Cream (37) |
Brown Rice—Calrose (87) |
|
Chocolate Milk with Sugar (34) |
Corn Thins (87) |
|
M&Ms with peanuts (33) |
Baked Potato (85) |
|
Pizza Supreme (30) |
Boiled Potato (101) |
|
Egg Fettuccine (32) |
Parsnips (97) |
|
Fructose—a pure sugar (19) |
Carrots (92) |
The concept of glycemic index was introduced by David Jenkins of the University
of Toronto in1981, and the vegetarian diets he and his fellow researchers used consisted of starches, vegetables, and fruits
that are low on GI scale, not the many “junk foods” that also have a low GI.2 (Please note that one
of the principal researchers from this University of Toronto group, Cyril Kendall PhD, will be a speaker at our next Advanced
Study Weekend, Sept. 29 to Oct. 1, 2006). Schedule
In the category of “healthy carbohydrates”: fruits, non-starchy
vegetables, nuts, and legumes tend to have a low GI. The GI of grains is variable, but typically high. Potatoes
and bananas (compared to other fruits) naturally have a higher GI..
|
What Does GI Measure?
Glycemic index (GI) measures the rise in blood sugar in a person
over the two to three hours following the consumption of an amount of food that contains 50 grams of carbohydrate. This
rise is then compared to a standard reference: the rise in blood sugar caused by consuming glucose (a  sugar) or white bread; also containing 50 grams of carbohydrate. The final result, the GI, is expressed as a percentage.
Meat, poultry, fish, cheese, and eggs do not have GI values themselves, because they contain little or no carbohydrate. sugar) or white bread; also containing 50 grams of carbohydrate. The final result, the GI, is expressed as a percentage.
Meat, poultry, fish, cheese, and eggs do not have GI values themselves, because they contain little or no carbohydrate.
In order to make the GI more relevant to daily eating, the concept of
“glycemic load” was introduced. Glycemic load figures in the actual amount of food consumed by multiplying
the GI of that food times the carbohydrate content of a typical-sized serving of the food. (Example: GI of a baked potato
= 85, times 30 grams of carbohydrate in a serving, equals a glycemic load of 26.) |
GI Overturns Nutrition Dogma
The findings from the GI demonstrate the falsity of the popular notion
that the rates of absorption are a matter of “simple carbohydrates” versus “complex carbohydrates.”
The gut is not a passive sieve that allows molecules to pass based on their size—rather it is an active
membrane with an “intelligence” that purposefully allows selected nutrients to enter at the correct rate and in
the correct amount. The large numbers of carbohydrates found in our foods have a wide variety of chemical compositions and
physical structures—as a result of complex interactions, they are digested and absorbed by the human small intestine
into the body at different rates—giving rise to diverse blood sugar and insulin responses.
GI Is Just One More Descriptive Quality of a Food
Foods are most often described based on their macronutrient content: like
low-carbohydrate, high-fat, high-protein, and low-fiber. The total calories in a serving of a food and cholesterol content
are also important descriptives. Some of the micronutrients, such as minerals (sodium, potassium, calcium, etc.), and vitamins
(B, C, E, etc.) are considered important enough to be verbally attached to a food, like calcium and milk, and iron and meat.
Foods are also described based upon how they function. The “satiety
index” describes the effect of a food on the appetite. For example, potatoes are found to be twice as satisfying
as meat or cheese.3 You want your foods to be satisfying. The rise in insulin in the blood after a
meal is measured as an “insulin score.” In this case, beef produces more insulin than whole wheat pasta,
and cheese more than porridge.4 Insulin drives fat into fat cells, so having a “high insulin
score” could be a disadvantage for a person trying to lose weight.
Low GI Diets Can Be Serious Health Hazards
Low GI does not necessarily equate to healthy food choices. The GI of
fructose is 19—about the lowest GI you can find. Table sugar (also known as white sugar and sucrose) is half fructose
(the other sugar in this disaccharide is glucose). About 55% of the sugar in high fructose corn syrup (HFCS) is fructose.
A diet full of sugar is one with a moderate GI. Every year people living in the USA consume, on average, 42.2 pounds
of HFCS (GI=60) and 45.2 pounds of table sugar (GI=68). In other words, every day they eat about one-quarter pound of
moderate GI food (these two kinds of sugars); which also translates into 500 “empty calories” consumed.
“Empty calories” in a food means no essential nutrients, like protein, essential fat, vitamins, minerals, or dietary
fiber, are present. Simple sugars, like white sugar and high fructose corn syrup, adversely affect the
action of insulin and cause weight gain and elevate triglycerides—all three factors increasing the risk of diabetes.
HFCS is believed to be a major player in the rising epidemic of obesity in Western societies.5
Focusing on a low glycemic index diet, while ignoring the other qualities
of a food, is also hazardous because the easiest way to decrease the blood sugar response (the GI) to dietary carbohydrate
is to consume more protein and fat—the predominant ingredients in meat, poultry, eggs, and cheese. As you know
well, these foods are well established to damage your arteries, bones, and kidneys—leading to heart attacks, strokes,
osteoporosis, kidney stones, kidney failure, and cancer.
GI Can Be an Impractical Tool
Many people stake their whole health future on the GI. However,
from the practical viewpoint of daily use, GI is too complex and changeable to precisely guide a person to the correct food
choices. Different studies find widely varying GI values; for example, sweet corn has been found to have a GI of 37, 46, 48,
59, 60, and 62.1 Cooking and cooling changes the food’s GI. The ripeness of the food increases the
GI. Disrupting a food’s dietary fiber by grinding, and also removing the fiber, make carbohydrates more easily
absorbed, increasing the GI. Mixing foods together results in a GI of the meal that cannot be predicted from the GI
of the individual foods. Therefore, even with great effort you will likely be way off your target GI.
High GI and Obesity
Over the past two decades, consumption of foods with high glycemic index
values have been associated with various chronic diseases, including type-2 diabetes, coronary heart disease, obesity, and
cancer. However, the data are far from clear and consistent—as a result, the usefulness of the GI for the treatment
of diabetes and obesity is debated. Some organizations like the Canadian Diabetic Association, consider this tool useful,
while the American Diabetic Association dismisses the value of GI in treating diabetes.6
Neither high nor low GI carbohydrates results in excess calorie consumption
or weight gain. In fact, a high-carbohydrate diet is crucial in preventing weight gain in those with a tendency for
obesity.7,8 Carbohydrate consumption promotes satisfaction of the appetite and higher GI foods do this even
better than low GI foods—because the elevation of the blood sugar after eating is one of the key mechanisms in satisfying
the appetite and reducing food intake.9 Worldwide, populations of hundreds of millions of people who eat
high GI potatoes (Peruvians) and rice (Asians) are trim and active for a lifetime. Compare this worldwide observation
to populations of obese people living in the USA, Australia, and Western Europe who feast daily on low GI sugars, fats, meats,
and cheeses.
Fat, Not Sugar, Causes Diabetes
According to a statement by the American Diabetes
Association, “…there is little evidence that total carbohydrate is associated with the development of type 2 diabetes.
Rather, a stronger association has been observed between total fat and saturated fat and type 2 diabetes.”10
Multiple studies have shown an inverse relationship between
the amount of carbohydrate consumed and the development of diabetes.11 Populations of people worldwide who eat diets centered on high glycemic index carbohydrates, like rice
for rural Asians, and potatoes for people in Peru, are essentially free of diabetes.12,13
|
Position statement of the American Diabetic Association14
“In subjects with type 2 diabetes, studies of 2–12 weeks duration
comparing low glycemic index and high glycemic index diets report no consistent improvements in HbA1c, fructosamine, or insulin
levels. The effects on lipids from low glycemic index diets compared with high glycemic index diets are mixed.” |
The reasons why carbohydrates benefit diabetics have their roots in our
fundamental metabolism. As far back as 1936 Harold Percival Himsworth reported that the ability of insulin
to lower blood sugar was improved by eating carbohydrates.15 In contrast, fats in the diet paralyze the activity
of insulin, cause insulin resistance, and cause the blood sugars to rise.11 All these changes, combined with
the resulting obesity from eating fatty foods, encourage the development of type-2 diabetes. For people now following the
Western diet, a change to a low-fat, high-carbohydrate diet slows progression to diabetes.16,17 This same
diet will cure type-2 diabetes.18-20
You Should Be a Seeker of Healthy High GI Foods
The primary purpose of eating is to replenish energy—this
is most efficiently accomplished thorough the assimilation of carbohydrates—high GI starches and vegetables do this
most rapidly. Carbohydrates from our foods pour into our bloodstream to become blood sugars. The brain, nervous
system, red blood cells, and kidney cells use only sugar for fuel (under duress the brain can burn fat). Twenty percent of
the body’s daily calorie intake goes to the brain, which means a lot of carbohydrate must appear in the bloodstream
after eating for this organ to perform efficiently. This is one reason low-carbohydrate diets, such as the one
recommended by Atkins, are associated with problems of brain function.21
“Carbohydrate loading” is a technique of eating which is employed
by all winning endurance athletes. Carbohydrates, stored as glycogen in the muscles and liver and later released into the
bloodstream, provide immediate energy for the whole body during a race. For the most efficient means of replenishing spent
glycogen reserves, athletes have learned to choose foods that have a high GI.22,23 Selecting foods with a
high GI is just as sound advice for anyone yearning to be strong and energetic throughout the day—not just for athletes.
Little Attention Should Be Given to the GI
Glycemic index is just another way to describe a functional affect of
foods on the body. Many popular diets, in particular those which promote high protein, high fat—meat and dairy—eating
have placed the GI above all else in their plans to help you lose weight. To ignore the overall qualities of food is
unwise. The high GI carbohydrates found in foods like a potatoes or carrots do not make them any more unhealthful than
do the simple sugars found in fruits make them unhealthful.
Nutrition-savvy people already know the general concept that legumes,
whole grains, fruits and vegetables are good foods. In the whole scheme of the nutritional needs of people the importance
of the rate of absorption of carbohydrates (the GI) is overrated and frequently leads the poorly-informed consumer to make
bad food choices.
References:
1) Foster-Powell K, Holt SH, Brand-Miller
JC. International table of glycemic index and glycemic load values: 2002. Am J Clin Nutr. 2002 Jul;76(1):5-56.
2) Jenkins DJ, Wolever TM, Taylor RH, Barker
H, Fielden H, Baldwin JM, Bowling AC, Newman HC, Jenkins AL, Goff DV. Glycemic index of foods: a physiological basis for carbohydrate
exchange. Am J Clin Nutr. 1981 Mar;34(3):362-6.
3) Holt SH, Miller JC, Petocz P, Farmakalidis E.
A satiety index of common foods. Eur J Clin Nutr. 1995 Sep;49(9):675-90.
4) Holt SH, Miller JC, Petocz P. An insulin
index of foods: the insulin demand generated by 1000-kJ portions of common foods. Am J Clin Nutr. 1997 Nov;66(5):1264-76.
5) Bray GA, Nielsen SJ, Popkin BM. Consumption
of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am J Clin Nutr. 2004 Apr;79(4):537-43.
6) Sievenpiper JL, Vuksan V. Glycemic index
in the treatment of diabetes: the debate continues. J Am Coll Nutr. 2004 Feb;23(1):1-4.
7) Jequier E, Bray GA. Low-fat diets are preferred.
Am J Med. 2002 Dec 30;113 Suppl 9B:41S-46S.
8) Saris WH. Glycemic carbohydrate and body
weight regulation. Nutr Rev. 2003 May;61(5 Pt 2):S10-6.
9) Anderson GH, Woodend D. Effect of glycemic
carbohydrates on short-term satiety and food intake. Nutr Rev. 2003 May;61(5 Pt 2):S17-26.
10) Sheard NF, Clark NG, Brand-Miller JC, Franz
MJ, Pi-Sunyer FX, Mayer-Davis E,
Kulkarni K, Geil P.Dietary carbohydrate (amount
and type) in the prevention and management of diabetes: a statement by the american diabetes association. Diabetes Care.
2004 Sep;27(9):2266-71.
11) Bessesen DH. The role of carbohydrates
in insulin resistance. J Nutr. 2001 Oct;131(10):2782S-2786S.
12) Kitagawa T. Increased incidence
of non-insulin dependent diabetes mellitus among Japanese schoolchildren correlates with an increased intake of animal protein
and fat. Clin Pediatr (Phila). 1998 Feb;37(2):111-5.
13) Llanos G. Diabetes in the Americas. Bull
Pan Am Health Organ. 1994 Dec;28(4):285-301.
14) American Diabetes Association. Evidence-based
nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes
Care. 2002 Jan;25(1):202-12.
15) Himsworth HP. Diabetes mellitus: its differentiation
into insulin-sensitive and insulin-insensitive types. Lancet 1936;i:127-130).
16) Kim SH, Lee SJ, Kang ES, Kang S, Hur KY, Lee
HJ, Ahn CW, Cha BS, Yoo JS, Lee HC. Effects of lifestyle modification on metabolic parameters and carotid intima-media
thickness in patients with type 2 diabetes mellitus. Metabolism. 2006 Aug;55(8):1053-9.
17) Kulkarni K. Diets do not fail: the success of
medical nutrition therapy in patients with diabetes. Endocr Pract. 2006 Jan-Feb;12 Suppl 1:121-3.
18) Kiehm TG, Anderson JW, Ward K. Beneficial
effects of a high carbohydrate, high fiber diet on hyperglycemic diabetic men. Am J Clin Nutr. 1976 Aug;29(8):895-9.
19) Jenkins DJ, Kendall CW, Marchie A, Jenkins
AL, Augustin LS, Ludwig DS, Barnard ND, Anderson JW. Type 2 diabetes and the vegetarian diet. Am J Clin Nutr.
2003 Sep;78(3 Suppl):610S-616S.
20) Nicholson AS, Sklar M, Barnard ND, Gore
S, Sullivan R, Browning S. Toward improved management of NIDDM: A randomized, controlled, pilot intervention using a
lowfat, vegetarian diet. Prev Med. 1999 Aug;29(2):87-91.
21) Wing RR. Cognitive effects of ketogenic
weight-reducing diets. Int J Obes Relat Metab Disord. 1995 Nov;19(11):811-6.
22) Hawley JA. Effect of meal frequency
and timing on physical performance. Br J Nutr. 1997 Apr;77 Suppl 1:S91-103.
23) Walton P. Glycaemic index and optimal
performance. Sports Med. 1997 Mar;23(3):164-72.
|


 Type-2 Diabetes: A Runaway Epidemic Caused by Rich Foods
Type-2 Diabetes: A Runaway Epidemic Caused by Rich Foods
 sugar) or white bread; also containing 50 grams of carbohydrate. The final result, the GI, is expressed as a percentage.
Meat, poultry, fish, cheese, and eggs do not have GI values themselves, because they contain little or no carbohydrate.
sugar) or white bread; also containing 50 grams of carbohydrate. The final result, the GI, is expressed as a percentage.
Meat, poultry, fish, cheese, and eggs do not have GI values themselves, because they contain little or no carbohydrate.